The keto diet (ketogenic diet) is one of many nutrition plans making headlines today.
Those who eat according to the keto diet follow a low carbohydrate plan mixed with moderate protein and high-fat, and the goal of the diet is to optimize the metabolic state of the body. Many experts now agree that the keto diet supports healthy insulin levels, boosts fat loss, increases metabolic health, promotes mental clarity, lowers inflammation, and more.
The keto diet was initially developed in the 1920s to help with central nervous system challenges in children. Doctors and researchers at the Mayo Clinic noticed their pediatric epileptic patients were having fewer seizures when they fasted. These findings inspired them to create a diet that mimicked starvation mode in a manner that could be sustained long-term.
The immune system is one of the many mechanisms in the body significantly impacted by dietary choices, and the keto diet has been shown to influence the immune system positively. In particular, the keto diet can support autophagy, an essential cellular renewal process that is inhibited by sugar, especially refined sugar. By reducing carbohydrates and sugar, an improved metabolic state works to improve gut health, promote autophagy, decrease insulin resistance, and elicit other immune-supporting responses.
What is the Keto Diet and Ketosis?
Ketones are created by the liver and can be used as an energy source in the body. Burning ketones for energy is a normal metabolic occurrence and was likely the body’s most preferred fuel source throughout human history. Consider our Paleolithic ancestors who lived off the land as an example. Food sources were only available intermittently, depending on the season, climate, and other factors. This means that our ancestors rarely indulged in carbohydrates and sugar as we do today, and it is unlikely that they regularly consumed multiple meals a day. As a result, their bodies operated within a necessary, natural state of ketosis.
Ketosis is a metabolic state that occurs as the number of ketones in the body increases. The keto diet triggers ketosis, and this process optimizes the fuel we burn from meals.
Fast-forward to today, and we find that an ordinary diet is filled with carbohydrates and processed and refined carbs. For many people, simple carbs and refined sugar serve as their primary fuel source, instead of protein and fat. This conventional diet assumes that glucose is a necessary and preferred fuel source for the body. For that reason, one must continually eat carbs to refill glycogen stores.
We now have a greater understanding that during ketosis, skeletal muscles and even the brain effectively use fat in the form of ketones for sustained energy. And this seems to be a more efficient, less detrimental fuel source.
Using fat for fuel creates far less oxidation and more energy than carbohydrates. Ketones also provide more energy per unit of oxygen used. Interestingly, being in the metabolic state of ketosis increases the number of mitochondria, which increases the potential energy-output of your cells.
Eating a low carbohydrate diet causes the body to depend on fat as the primary fuel source, decreasing glucose oxidation. This ultimately helps to regulate the body’s inflammatory inflammation and keep inflammation within normal levels. Many studies have concluded that systemic inflammation is a contributor to several health problems, and decreasing it is key to health and longevity.[1]
What Can You Eat on a Keto Diet?
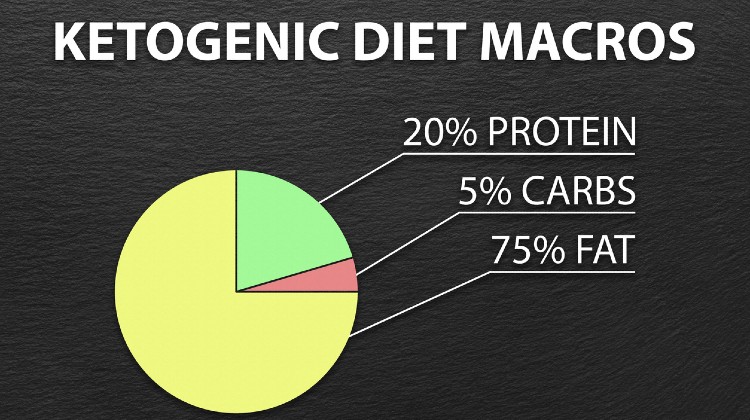
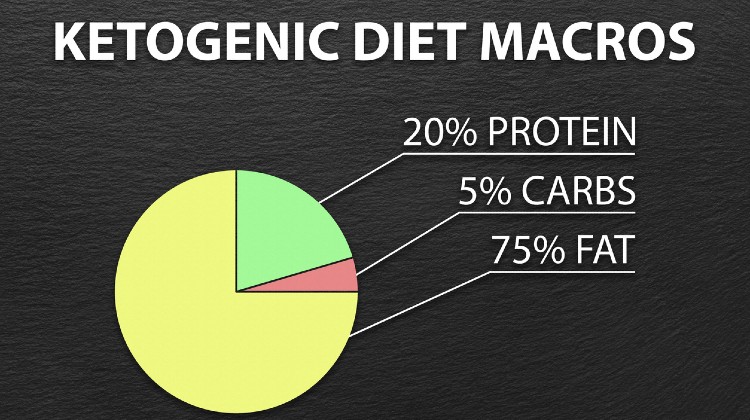
The guidelines for the keto diet includes getting about 75% of your calories from fat, 20% from protein, and 5% from carbohydrates. A keto plate includes non-starchy vegetables (leafy greens, broccoli, cauliflower, green beans, etc.), healthy fats like olive and coconut oil, avocado, nuts and seeds, and protein from meat, fish, eggs, and dairy.

How Does Keto Impact the Immune System?
The keto diet impacts the immune system in a number of ways, perhaps most notably by triggering the release of a ketone called beta-hydroxybutyrate (BHB), which is known to decrease cellular damage from outside invaders by helping to maintain a healthy inflammatory response.* The keto diet is highly effective in regulating inflammation, and BHB seems to be one of the primary reasons why.*
Studies also suggest that a ketogenic diet can change the gut microbiome for the better, decreasing instances of leaky gut and balancing gut flora. A well-functioning gut microbiome is key to a well-functioning immune system, so the keto diet impacts immune function in this way as well.[2]
High blood sugar and poor insulin sensitivity can also increase the risk for many health issues. A keto diet can improve insulin sensitivity and decrease resistance, thereby supporting the immune system as well.[3]
Autophagy is another factor at play. We could think of autophagy as the body’s innate cellular clean-up crew, wiping out waste and toxins the body no longer needs. If waste and toxins build up over time, cell function degrades and declines, potentially leading to weight gain, low energy, increased inflammation, and other health challenges. Fasting has been found to induce autophagy, and the keto diet activates some of the same pathways in the body that fasting does, such as the 5' adenosine monophosphate-activated protein kinase (AMPK) pathway.[4]
If It’s an Immune Booster, What is the Keto Flu?
The term keto flu is somewhat of a misnomer, as it has no relation to a viral or bacterial illness. However, keto flu is a term used to describe the sluggish feeling that can occur when the body enters ketosis. Dietary supplements and other small changes can help limit the negative effects associated with transitioning to the ketogenic diet.*
Keto-flu may present as headaches, muscle cramps, constipation, bloating, or dizziness. Whether or not you will experience keto flu symptoms depends on many individual factors such as diet history, health status, genetics, hormones, and more.
Transitioning from a very high-carb diet to a keto diet too quickly can also trigger flu-like symptoms or make them worse. This is why it’s important to slowly transition into the keto diet, moving first from refined foods to whole foods carb sources, and then slowly lowering the total amount of carbs overall. Intentionally monitoring the pace at which you transition to keto can greatly reduce unpleasant experiences along the way. Increasing electrolyte intake can also help to reduce the likelihood of keto flu.
Supplementing your diet with exogenous ketones, like BHB may help limit the uncomfortable experiences associated with transitioning to the keto diet.* BHB supplementation allows your body to skip a couple of steps in the Kreb cycle (part of the ketosis process), helping to make the transition to a keto diet more manageable.*
Can a Bad Diet Affect Your Immune System?
Sodas, candy, high fructose corn syrup, and other refined sugars are known to upregulate inflammatory pathways. Several studies have concluded that a diet high in processed sugar leads to dysregulated blood sugar, lowered insulin sensitivity, problems with gut permeability, and poor inflammatory response.[5]
A study of 29 healthy adults found that after consuming 40 grams of added sugar from one can of soda per day resulted in a significant increase in inflammatory markers such as LDL cholesterol.[6] Sugar also directly impacts the immune system by lowering the efficacy of white blood cells for as long as 1-2 hours after ingestion.[7]
Along with sugar, other immune offenders include smoking, alcohol, a sedentary lifestyle, and frequent stress.
Conclusion
Taking steps to improve your immune system can help increase energy, manage weight, prevent future health problems, and promote an overall healthier life. The ketogenic diet naturally facilitates improved immune function with a diet rich in whole foods, green vegetables, plenty of proteins, and healthy fats to regulate glucose. Overall, the keto diet encourages the body to utilize a cleaner fuel source that does not depend on a constant influx of carbs and insulin.

[1] Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., Ferrucci, L., Gilroy, D. W., Fasano, A., Miller, G. W., Miller, A. H., Mantovani, A., Weyand, C. M., Barzilai, N., Goronzy, J. J., Rando, T. A., Effros, R. B., Lucia, A., Kleinstreuer, N., & Slavich, G. M. (2019). Chronic inflammation in the etiology of disease across the life span. Nature medicine, 25(12), 1822–1832. https://doi.org/10.1038/s41591-019-0675-0
[2] Reddel, S., Putignani, L., & Del Chierico, F. (2019). The Impact of Low-FODMAPs, Gluten-Free, and Ketogenic Diets on Gut Microbiota Modulation in Pathological Conditions. Nutrients, 11(2), 373. https://doi.org/10.3390/nu11020373
[3] Hu, T., Yao, L., Reynolds, K., Whelton, P. K., Niu, T., Li, S., He, J., & Bazzano, L. A. (2015). The Effects of a Low-Carbohydrate Diet vs. a Low-Fat Diet on Novel Cardiovascular Risk Factors: A Randomized Controlled Trial. Nutrients, 7(9), 7978–7994. https://doi.org/10.3390/nu7095377
[4] Paoli, A., Bosco, G., Camporesi, E. M., & Mangar, D. (2015). Ketosis, ketogenic diet and food intake control: a complex relationship. Frontiers in psychology, 6, 27. https://doi.org/10.3389/fpsyg.2015.00027
[5] Frazier TH, DiBaise JK, McClain CJ. Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. JPEN J Parenter Enteral Nutr. 2011 Sep;35(5 Suppl):14S-20S. doi: 10.1177/0148607111413772. Epub 2011 Aug 1. PMID: 21807932.
[6] Aeberli I, Gerber PA, Hochuli M, Kohler S, Haile SR, Gouni-Berthold I, Berthold HK, Spinas GA, Berneis K. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am J Clin Nutr. 2011 Aug;94(2):479-85.
[7] Albert Sanchez, J. L. Reeser, H. S. Lau, P. Y. Yahiku, R. E. Willard, P. J. McMillan, S. Y. Cho, A. R. Magie, U. D. Register, Role of sugars in human neutrophilic phagocytosis, The American Journal of Clinical Nutrition, Volume 26, Issue 11, November 1973, Pages 1180–1184, https://doi.org/10.1093/ajcn/26.11.1180











.jpg)

-1.jpg)




